Call Now
Dr. Jacques Fontaine and the world’s leading esophageal cancer experts at Moffitt Cancer Center provide extensive and individualized treatment options for those with this rare malignancy. Patients at Moffitt have access to the latest techniques in surgery, chemotherapy and radiation.
Treating Esophageal Cancer
The most effective therapy options for esophageal cancer patients are surgery, chemotherapy and radiation. The stage of your cancer will determine which treatment options are available. Moffit’s medical team will customize the appropriate treatment based on your test results.
The team will discuss your plan with you after they have determined your cancer type and stage. In many cases, treatment plans associated with the highest survival rates and most significant improvement to quality of life will consist of a combination of therapies such as chemotherapy and radiation.
How Stages of Esophageal Cancer Affect Treatment
Primary treatment options for esophageal cancer differ by stage. Fontaine and Moffitt’s team of experts will discuss your case in a multidisciplinary tumor board and determine the best course of treatment for you. Treatments will vary based on whether your cancer is in early, intermediate or late-stage disease.
-
Stage I (Early stage): An esophagectomy removes the esophageal cancer through surgery and offers the best chance for a cure. This procedure does not require follow-up chemotherapy or radiation. In some cases, your surgeon can use a technique called endomucosal resection to shave off very thin tumors without traditional surgery.
-
Stage II/III (Intermediate stage): The best treatment option for intermediate stage esophageal cancer is to shrink tumors through a combination of six weeks of chemotherapy and radiation followed by surgical removal. In 10% of patients, cancer may spread after the initial therapy and surgery is not advisable for a cure.
-
Stage IV (Advanced stage): Surgery is not an option if the tumor has metastasized to other areas or organs. The recommended option is chemotherapy alone, which may shrink and slow the growth of cancer. The chance of a cure in this situation is slim, but chemotherapy allows patients to live longer and more easily swallow food.
Esophageal Cancer Surgery and Treatments
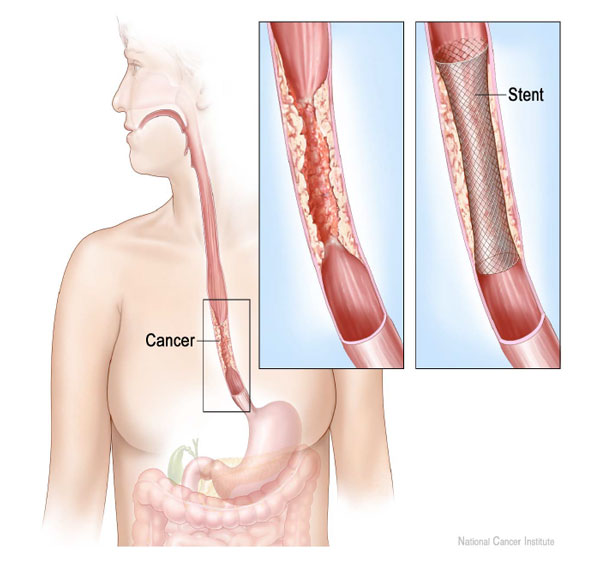
The primary surgical option for esophageal cancer patients is the Ivor Lewis esophagectomy. This procedure removes most of the esophagus and involves a lengthy recovery. Some patients may receive an esophageal stent that prevents obstruction and improves swallowing.
Before undergoing surgery, most patients receive weekly chemotherapy and daily radiation over six weeks. This upfront treatment shrinks the tumor and makes it more likely for the thoracic surgeon to eradicate it. It also decreases the risk of cancer recurrence after surgery.
Chemotherapy and Radiation
For patients with intermediate-stage esophageal cancer, a combination of six weeks of chemotherapy and radiation is the best treatment option. Most patients receive weekly chemotherapy and 28 daily radiation doses across six weeks to shrink tumors for complete removal during surgery.
Patients take about eight weeks to recuperate from treatment. Afterward, they will undergo a repeat PET scan to assess if the tumor responded to treatment. Chemotherapy and radiation typically begin within two weeks of initial diagnosis. If you are eligible for surgery, your doctor will schedule the procedure about a month after the repeat PET scan.
In some instances, after initial chemotherapy and radiation, the tumor may seem to have disappeared entirely on a repeat PET scan or endoscopy. Although tumors may not be visible on tests, microscopic tumor cells are still present and alive in more than 70% of cases. Therefore, all patients must be physically and mentally prepared to undergo surgery after chemotherapy and radiation.
Because cancer can spread via a process called metastasis, patients should not wait for tumors to return before deciding to have surgery. Additionally, the risk of complications from delaying surgery is much higher because of the long-term effects and scar tissue from radiation therapy. However, esophagectomy may not be advisable if patients have not fully recovered from the initial six weeks of chemotherapy and radiation.
Esophagectomy
An Ivor Lewis esophagectomy is a high-risk surgical procedure that takes six hours and removes two-thirds of the esophagus and the surrounding lymph nodes. After your surgeon removes the cancerous section of your esophagus, the stomach will be shaped into a cylinder and pulled higher into the chest. Then, your surgeon will connect the stomach to the remaining esophagus in the upper chest.
Fontaine and his colleagues at Moffitt Cancer Center are leaders in esophageal cancer surgery, performing more robotic esophagectomies than any other center in the United States. Minimally invasive or robotic surgery offers many advantages, including fewer complications, less trauma and blood loss and decreased pain.
Robotic surgery involves just a few small cuts performed by your surgeon with the aid of a magnifying 3D camera and miniaturized, precise instruments. Most complications from the surgery are minor and temporary. The recovery period is long and can be challenging. However, this surgery offers the best chance of a cure.
Patients typically stay in the hospital about a week after an esophagectomy, but recovery may take up to six months. Some patients experience fatigue, poor appetite, diarrhea, reflux or vomiting, but these symptoms usually improve over time. Post-surgical patients should walk for 20 minutes twice a day and remain active. Once fully recuperated, patients may return to a regular diet and resume their everyday activities.
Esophageal Stent Placement
An obstructed esophagus can cause pain while eating and increase the risk that food refluxes back up from the stomach. Your doctor may recommend placing an esophageal stent within your esophagus to open a blocked area. The stent is a plastic or metallic cylinder that helps you swallow foods and liquids.
During the procedure, you will receive anesthesia so that you are asleep and feel no pain. The surgeon then introduces a long, thin tube called a catheter into your esophagus through the mouth.
Once in position, your surgeon places the folded stent over the catheter and moves it to the area of blockage. The stent opens and pushes against the walls of the esophagus, providing support and space for swallowing. After placement, the surgeon removes the catheter.
Medical staff should clear you to go home the same day. You will need someone to drive you home and will receive instructions for a strict diet. In some cases, you may need to stay overnight in the hospital.
An esophageal stent procedure has relatively minor risks, but complications may arise later. Common problems include:
-
Pain or mild bleeding in the esophagus
-
Stent movement out of position
-
Gastroesophageal reflux (heartburn)
In some cases, patients may require a repeat procedure due to complications. Risks will vary based on overall health, the extent of esophageal blockage and the type of stent used.
Dietary Guidelines Following Esophageal Stent Placement
The esophageal stent can become clogged if you attempt to eat foods that are hard or sticky. If your stent becomes clogged, obstructed or otherwise unusable, this is a severe problem that may require surgery. Following a specific diet decreases the risk of stent blockage.
General guidelines include:
-
Chew all foods thoroughly.
-
Eat five to six small meals per day if needed.
-
Eat slowly and take small bites.
-
Sit upright when eating.
-
Drink a small amount of fluid after every two to three bites.
-
Prepare all foods so that they are moist, soft and easily swallowed.
If food ever feels “stuck” in your throat or chest, take a few sips of soda or any carbonated drink, which will help dislodge the food from your esophagus. If you are having trouble maintaining your weight, you may need to add calories by drinking nutritional supplements.
Commercial Nutritional Supplements
Dietary supplements include nutrients and extra calories in addition to your modified diet. Many of the following options come in multiple flavors and are easy to swallow after your procedure. To make a milkshake, try blending these products with ice, ice cream, sherbet or sorbet.
-
Boost
-
Ensure
-
Kroger Fortify (Kroger brand)
-
Equate (Walmart brand)
-
Nutra-Shakes (1-800-654-3691)
-
Carnation Instant Breakfast (made with whole milk)
The following chart of recommended foods will help guide you toward healthy and safe options after your esophageal stent procedure. For each food group, you should prioritize foods in the “YES” column over foods that are labeled “AVOID.” By adhering to these guidelines, you will minimize your risk of esophageal stent complications.
Eating Guide for Esophageal Stent Surgery Patients
| FOOD GROUP | YES FOODS | AVOID |
|---|---|---|
| Milk and Dairy Products | Milk — all kinds, yogurt, custard, ice cream, soft or melted cheese, cottage cheese, cream cheese | Ice cream or yogurt with chunks of fruit or nuts |
| Meat and Meat Substitutes | Soft eggs, tofu, casseroles, moist fish, strained baby meats (for easy preparation). All other meats must be bite-sized or ground — suggest adding a gravy or sauce | Dry poultry, peanut butter, all tough red and white meats |
| Fruits | All juices, all canned fruits, fresh fruits peeled — bananas, stewed dried fruits | Fresh fruits with skins — plums, peaches, oranges, apricots. Dried fruits |
| Vegetables | Well-cooked soft or pureed, should be “fork-tender,” strained baby vegetables | Raw vegetables |
| Bread and Starchy Foods | Cooked cereal, mashed potatoes, sweet potatoes, yams, baked potato without skin, soft moist rice, noodles, macaroni, spaghetti, dry cereals softened in milk, pancakes softened with syrup/butter, waffles softened with syrup/butter, crackers or breads added to soups | Hard bread with thick crust, dry cereals without milk, potato chips, popcorn, crackers |
| Fats | Butter, margarine, mayonnaise, salad dressings, gravy, cream: sour, whipping, coffee | Bacon, nuts, deep fried, crispy food |
| Desserts | Sherbet, ice creams, Italian ice, frozen yogurts, gelatin, puddings, mousse, custard, all cake-type desserts | Cookies, pie crust, any dry desserts, desserts containing nuts or skins |
| Other | Sauces — cheese, white, barbeque, creamed, tomato. Syrup, honey, jam, jelly, ketchup, mustard, relish |